Coming soon
Strengthening national systems, empowering communities, and sharing real stories—this book celebrates inclusive, sustainable NCD care in Jordan and Lebanon amid immense challenges.
Strengthening national systems, empowering communities, and sharing real stories—this book celebrates inclusive, sustainable NCD care in Jordan and Lebanon amid immense challenges.
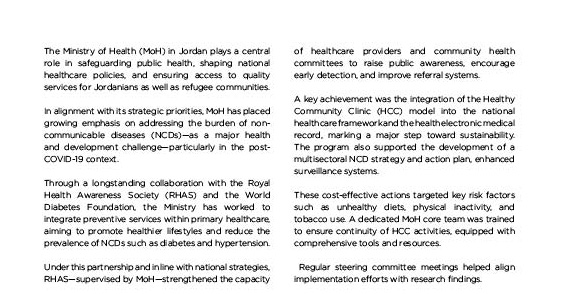
Jordan and Lebanon are among the countries with the highest number of refugees per capita in the world. Both nations had already been facing a significant burden of NCDs, with conditions such as diabetes and hypertension accounting for the majority of preventable illness and death.
Their health systems—largely focused on primary care—were already under strain. The arrival of large numbers of displaced people, many of whom were also living with NCDs, added further pressure and exposed critical gaps in prevention, diagnosis, and long-term care. What followed was not the adoption of a new model, but the expansion of an existing one—a scaled, integrated approach that sought to strengthen national systems while improving access to care for both refugee populations and host communities.
The WDF, with co-funding from the Novo Nordisk Foundation (NNF), together with long-standing WDF partners, saw the necessity to form a response to this immense challenge. Collaborating closely with longstanding local partners and spearheaded by the Ministry of Health (MoH) in Jordan and the Ministry of Public Health (MoPH) in Lebanon, the partners launched two separate national initiatives—one in Jordan and one in Lebanon.
The objective was both clear and ambitious: integrate NCD care into national healthcare responses, make services more inclusive of the vulnerable host community and refugees, and resilient, demonstrate what can be achieved when systems are strengthened rather than replaced by parallel systems, leading to more equitable, resilient, and sustainable healthcare systems.
This book chronicles that response.
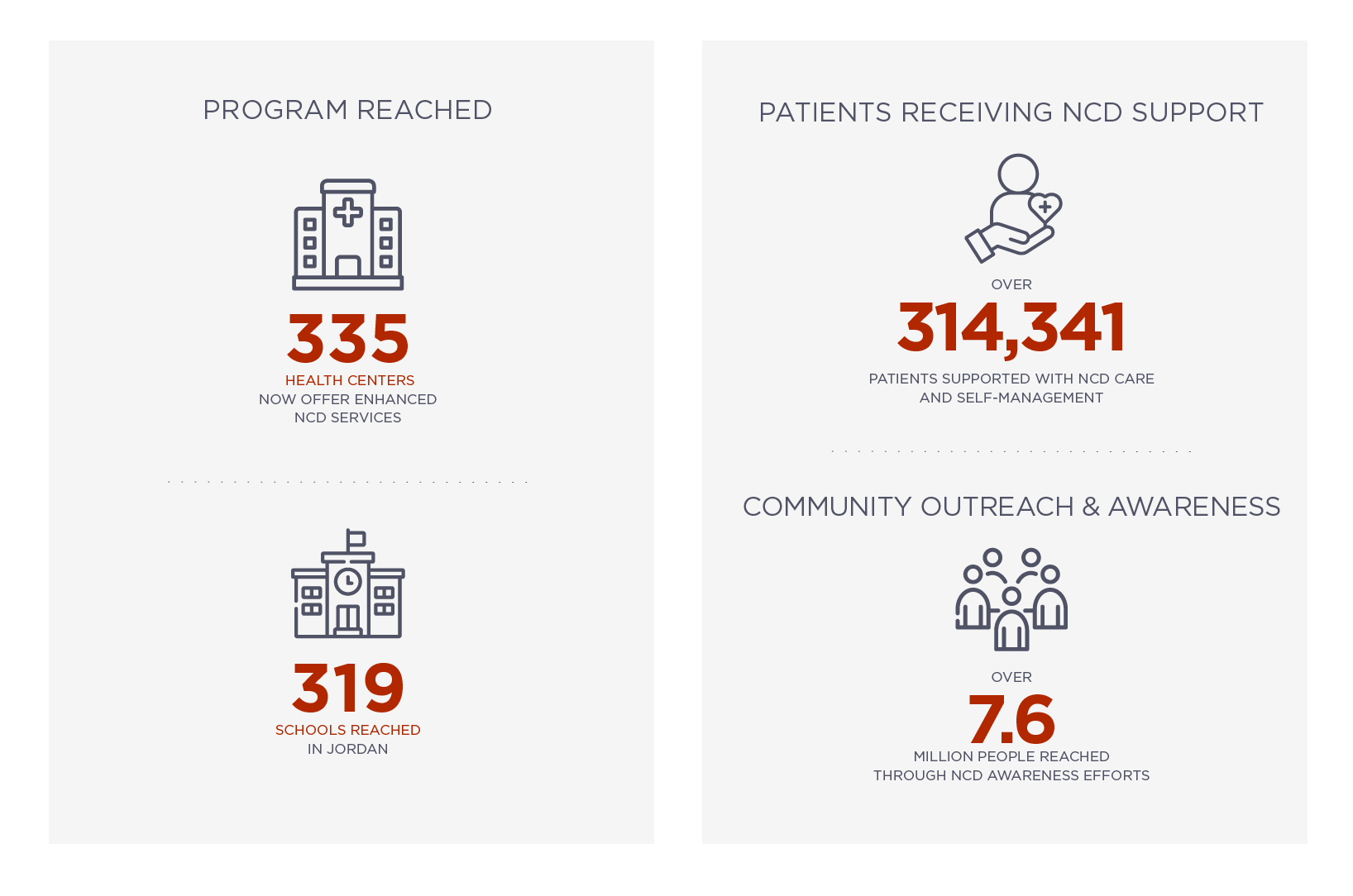
In Jordan, the initiative began in 2020, during the onset of the COVID-19 pandemic. Designed in collaboration with the MoH and led on the ground by the Royal Health Awareness Society (RHAS), the initiative focused on strengthening NCD prevention and care through an integrated, system-wide approach.
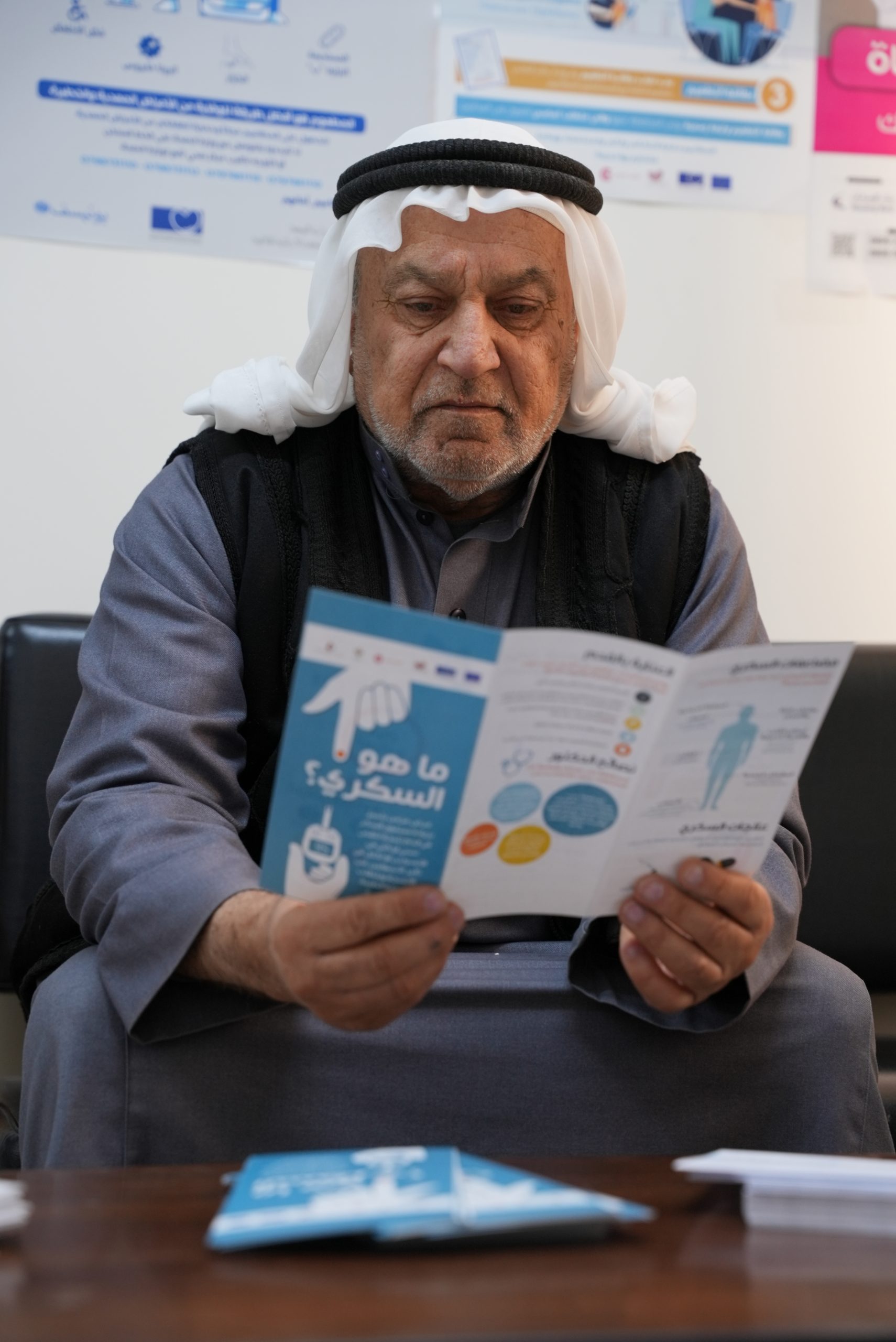
The programme centred on expanding services at primary healthcare centres, improving access to early detection and counselling, and promoting healthier lifestyles through community and school-based engagement. Activities included the revitalisation of the Healthy Community Clinics Programme, capacity-building for healthcare providers, and targeted outreach to vulnerable populations in host communities and refugee camps.
A key component of the initiative was its focus on youth—delivered through an expanded Healthy Schools Programme—which marked the first time a national NCD initiative in Jordan had integrated young people at such scale.
In Lebanon, a complementary approach was launched in 2021, in partnership with the MoPH and the American University of Beirut (AUB). The broader initiative was divided into two tracks: a community-led response implemented by the Danish Refugee Council, and a health centre-based intervention carried out with MoPH and AUB.
This book focuses on the latter—chronic care strengthening delivered through MoPH-affiliated primary healthcare centres. The intervention aimed to improve the quality of NCD services in more than 100 primary healthcare centres by strengthening provider training, updating clinical protocols, introducing facility-level data tools, and supporting institutional development.
In both countries, activities were deliberately embedded within existing public health frameworks, helping to build national capacity, strengthen service delivery, and expand access to chronic disease care for both refugee populations and host communities. This system-based approach ensured that improvements were not only inclusive but positioned for long-term sustainability.






qwertyuio





qwertyuio
As the interventions in Jordan and Lebanon continue to unfold, they offer more than a retrospective of what has been achieved—they offer a vision for what is possible. They stand as a reminder that chronic disease care is not a luxury reserved for stable settings. It is a necessity—one that becomes even more urgent during times of crisis.
What has taken root in both countries is not just a series of services, but a shift in mindset. NCD prevention and management are now more deeply embedded within national health agendas. Health centres are better prepared to identify and support people living with chronic conditions. Training systems have been formalised. Data flows more efficiently. And perhaps most importantly, a growing number of patients are receiving care that is structured, consistent, and rooted in dignity.
Still, the work is not finished. In Lebanon, where the intervention is ongoing, the focus must remain on expanding reach, reinforcing policy, and continuing to build institutional capacity. The systems and tools that have been introduced are laying the foundation for long-term resilience, but they will require continued support to reach their full potential.
In Jordan, the opportunity now lies in scale and replication. The model developed through the intervention has already been institutionalised within the MoH. Its success offers a blueprint for future programmes—within the country and beyond. Further investment could extend its reach, deepen its integration, and ensure that it remains a living part of the national health system.
Across both contexts, the path forward depends on sustained commitment—not just from ministries or funders, but from the broader health and humanitarian communities. Chronic care must be recognised as a core element of health equity, particularly in fragile settings where people are at greater risk of being left behind.
The response led by WDF and its partners has already demonstrated what this kind of commitment can achieve. It has shown that even in times of crisis, systems can be strengthened, communities can be empowered, and lives can be changed. It has created not just results—but momentum.
Now is the time to build on that momentum. To continue supporting national systems. To keep investing in people. And to ensure that inclusive care is not the exception, but the expectation—wherever it is needed most.


qwertyuio








